Abstract
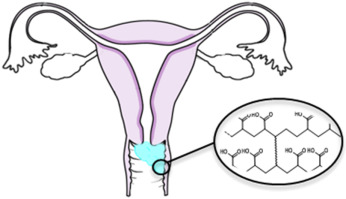
Intravaginal drug delivery can elicit a local effect, or deliver drugs systemically without hepatic first pass metabolism. There are a number of emerging areas in intravaginal drug delivery, but the vagina is a challenging route of administration, due to the clearance mechanisms present which result in poor retention of dosage forms, and the potential for irritation and other adverse reactions. Gel formulations are desirable due to the ease of application, spreading and that they cause little to no discomfort to the patient. However, these dosage forms, in particular, are poorly retained and traditional gels typically have little control over drug release rates. This has led to a large number of studies on improving the retention of vaginal gels and modulating the controlled release of drugs from the gel matrix.
This review outlines the anatomy and physiology of the vagina, focussing on areas relevant to drug delivery. Medical applications of vaginally administered medicines is then discussed, followed by an overview of polymeric gels in intravaginal drug delivery. The sensorial properties of intravaginal gels, and how these relate to user compliance are also summarised. Finally, some important barriers to marketing approval are described.
Conclusions
Vaginal drug delivery offers many opportunities for novel treatments of local disease, and for systemic drug delivery. It is, however, a difficult route of administration due to its sensitivity and the difficulty in retaining dosage forms. Gel formulations currently in use offer ease-to-use treatments for a variety of conditions, and recent advances in the area of pre-exposure HIV prophylaxis has increased interest in vaginal delivery. Users of vaginal gels often complain of messiness and leakage, which reduces their adherence to a treatment regimen, thus lowering efficacy. Sensory evaluation of vaginal gels is therefore crucial before clinical trial takes place, in order to ensure adherence to treatments. Efforts to improve the retention of vaginal medicines involves the incorporation of “mucoadhesive” excipients or the thickening of gels within the vagina, using pseudoplastic or thixotropic gel systems which shear-thin during application, or using thermogelling materials, which increase in viscosity after warming in the vagina. Synthetic materials have been created to enhance mucoadhesion and retention in the vagina, however these polymers have not yet been approved for use in humans and there is a greater need for researchers to consider the toxicity and irritancy of these products during their design. In particular, irritation of the vaginal mucosa has been a significant issue in PrEP research, enhancing HIV transmission.